When to use Antibiotics
What are antibiotics?
Most people have a general understanding of antibiotics: they get rid of bacteria in your body that contribute to infections.There are many different types of antibiotics that work in different ways on different bacteria to fight infections. Antibiotics can be bacteriostatic (limiting bacterial growth) or bactericidal (killing bacteria).
Although antibiotics can be an effective and even life-saving treatment for bacterial infections, there are important rules for how and when they should be used. Unfortunately, if these rules are not followed, antibiotic resistance can develop. This means that the bacteria becomes resistant and the antibiotics used against them are no longer effective. This makes it challenging when trying to treat infections caused by antibiotic resistant bacteria.
Another area to watch out for when you are prescribed antibiotics is your microbiome health. Imbalances in the bacteria in your intestines can lead to Clostridium difficile infections. Often probiotics are prescribed in conjunction with antibiotics in order to protect the delicate balance of the microbiome that determines gut health. Feel free to ask one of our MedinAction doctors or your provider about your intestinal health and the use of probiotics when you are prescribed antibiotics.
When should I be prescribed antibiotics?
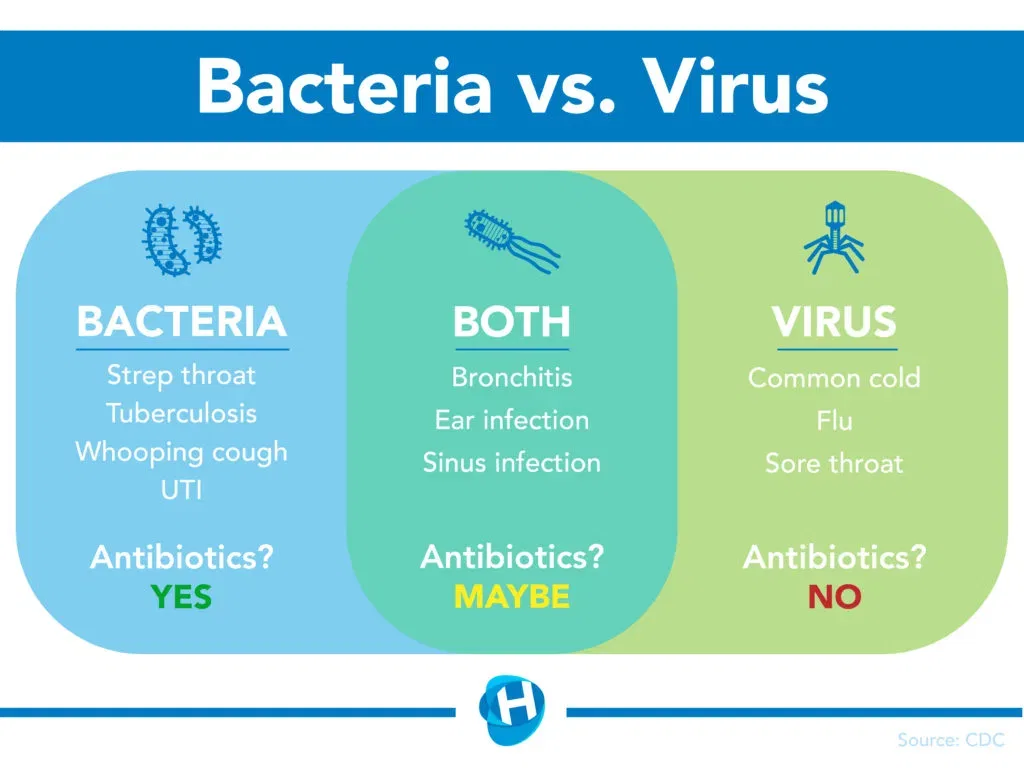
Antibiotics are useful against bacteria, not viruses. This may seem like common sense, but many patients go to a healthcare provider when they are sick and expect to be given antibiotics as a “quick fix” for their infections.
Your doctor often can diagnose you through a medical history and physical exam. In some cases, your doctor may need to do a culture like a throat swab, blood or urine test. The first step is to contact MedinAction or your healthcare provider if you believe that you have one of these conditions! The doctor can help determine what type of infection you have and the proper treatment.
According to health.com most doctors consider four things when faced with a virus vs. bacteria question:
- Have a fever? Common with both bacterial and viral illnesses. But if the flu is circulating in your area right now, antibiotics won’t be the answer to the virus. Your doctor will look to treat your symptoms. Be sure to get a flu shot next season, if possible.
- Been sick long? Viral infections that linger sometimes can turn into a larger problem, such as a sinus infection when bacteria join in. Your doctor may prescribe an antibiotic.
- What color is it? While green or yellow mucus can be a sign of a bacterial infection, doctors say that’s an unreliable indicator of the need for an antibiotic.
- What’s your throat look like? White spots can be a sign of bacteria. A sore throat without other cold symptoms can be strep throat, which absolutely requires antibiotics. To be sure, you need a culture or rapid antigen test, which can be done while you wait.
So I’ve been prescribed antibiotics. What now?
It is very important that you take your antibiotics as prescribed. Taking a previously prescribed antibiotic, someone else’s prescription, too much or not enough of your prescription, or taking the antibiotic at the incorrect time can all lead to antibiotic resistance and/or other infections. Make sure to take your full prescription even if you start to feel better sooner.
As with any medication, allergies to and side effects from antibiotics may occur. It is very important to contact your healthcare provider if you have any symptoms of an allergic reaction- rash, hives, itching, watery eyes, stuffy nose, fever, swelling (including the tongue/throat), and/or trouble breathing. Allergies to medications can be life-threatening if not treated appropriately.

What is antibiotic resistance?
Antibiotic resistance occurs when bacteria are able to adapt to antibiotics so that the medications are no longer effective against the bacteria. This can be through gene mutation within the species of bacteria or from bacteria passing drug-resistant genes to other species. Either way, the original antibiotics used against the bacteria are no longer effective. Antibiotic resistance occurs in both agriculture and humans. It poses many issues for disease treatment. Healthcare workers may not be able to cure a patient’s infection when there are no antibiotics to stop the bacteria, which can lead to death.

Some examples of antibiotic resistant bacteria include:
-
- Staphylococcus aureus (MRSA)
- Clostridium difficile (C. diff- discussed in the next section!)
- Escherichia coli (E. coli)
- Enterococcus species (VRE)
- Neisseria gonorrhoeae
- Pseudomonas aeruginosa
- Mycobacterium tuberculosis
- Klebsiella pneumoniae
- Streptococcus pyogenes
How can I help limit antibiotic resistance?
There are multiple ways in which you can help stop the development and spread of antibiotic resistant infections. The best and easiest way is to prevent getting sick in the first place. Get vaccinated, practice safe food handling, and wash your hands! Limiting infection in the first place reduces antibiotic prescriptions and the spread of antibiotic resistant bacteria. If you do happen to get sick, cough and sneeze into your elbow and stay home to prevent spreading the infection to others.
Here are some of the ways you can help limit antibiotic resistance:
- Prevent infection to begin with (proper hygiene, vaccinations, safe food prep, etc.)
- Do not pressure your provider to prescribe you antibiotics when you are sick. Your doctors and nurses will give them to you at the proper times.
- Follow the directions for your antibiotic prescription:
- Take all the medication given to you in your prescription
- Even if you start to feel better, it is still important that you finish your prescription
- Do not take leftover antibiotics- they may be the wrong ones and you should have finished them when they were first prescribed
- Do not skip doses
- Take your doses at the correct time
- Do not take another person’s antibiotic prescription
- Do not give your antibiotics to other people
By following your healthcare provider’s directions and preventing the spread of infection, we all can help limit antibiotic resistance!

Gut Health, what does it mean ?
Although most people associate bacteria with sickness and infection, our bodies are composed of around 10 bacteria cells for every 1 human cell according to Scientific American. What you see in the mirror can be said to be 90% bacteria and 10% human in terms of cells! These bacteria perform many functions that keep us healthy. They help us digest food, fight off disease-causing bacteria, and even regulate hunger and levels of inflammation!
Clostridium difficile
As discussed above, our microbiome accomplishes many functions vital to our health. However, imbalances in the “good” and “bad” bacteria in our bodies can lead to infections and other conditions. One of these infections is caused by Clostridium difficile, commonly referred to as C. diff. A common cause of this infection is antibiotic use. The antibiotics can change the balance of bacteria in our intestines, leading to too many C. diff bacteria and infection. This type of infection leads to watery diarrhea, abdominal cramps and pain, tachycardia (feeling like your heart is racing), fever, nausea, and/or bloody or mucousy stools.
It is very important to contact MedinAction or your healthcare provider if you have these symptoms. C. diff infections can lead to dehydration and fluid/electrolyte imbalances, kidney issues, and even death.
To prevent C. diff infections, proper hand hygiene and antibiotic use is key. The bacteria produces spores that are very hard to kill. Therefore, hand sanitizer is not enough in this case and you need to wash your hands with warm water and soap to get rid of the spores. The spores are temperature resistant, but the act of washing your hands scrubs them off your skin.
What are other problems caused by microbiome imbalances?
Imbalances in intestinal bacteria have also been connected to psychiatric, neurological, metabolic, autoimmune, and intestinal disorders. See the picture below for specific examples.

Want to maintain or improve your gut microbiome health? Ask your healthcare provider about probiotic foods and supplements when you are prescribed an antibiotic. Kimchi, cultured foods (cheese and yogurt), and foods high in omega 3 fatty acids (salmon, walnuts, chia seeds) are all great options for keeping your intestinal bacteria in balance! For more information about probiotics, see our MedinAction blog post and other resources:
- Healthy Gut, Healthy Life– MedinAction
- The Cleveland Clinic
- The National Institutes of Health
- UK’s National Health Service
Ask for an advice from an expert. Insert your data, you will be contacted shortly!
[wpforms id=”14577″ title=”false” description=”false”]



